Predictive Biomarkers: Driving Precision Medicine in Oncology & Beyond
In the era of precision medicine, predictive biomarkers are revolutionizing how diseases are diagnosed, treated, and managed. These biological indicators help identify which patients are most likely to respond to specific therapies, reducing trial-and-error treatments and improving outcomes. While predictive biomarkers have transformed oncology—guiding targeted cancer therapies—they are also making waves in neurology, cardiology, and autoimmune diseases. From genetic mutations to protein expressions, these markers are shaping the future of personalized healthcare.
In this blog, we’ll explore how predictive biomarkers drive innovation in oncology and beyond and the challenges in their discovery and validation.
What is Biomarker Discovery?
A biomarker is a measurable biological characteristic that indicates disease risk, treatment response, or progression. There are several types of biomarkers, including diagnostic, monitoring, predictive, prognostic, and more. In modern medicine, professionals utilize analytical technology to measure a large number of biomarkers present in the human organism (in urine, hair, blood, tissues, etc.).
There are several steps included in biomarker discovery and validation:
- Identification: Researchers collect biological samples (e.g., blood, tissue, urine) and use techniques like genomics, proteomics, or metabolomics to identify potential biomarkers.
- Validation: The identified biomarkers are tested in different sample sets to confirm their reliability and consistency.
- Qualification: The biomarkers are evaluated in clinical studies to determine their relevance to a disease or condition.
Regulatory Approval & Implementation: If successful, the biomarker undergoes regulatory review and can be used in diagnostics, treatment monitoring, or drug development.
What Are Predictive Biomarkers?
A predictive biomarker is measured before treatment, and it’s a characteristic that identifies individuals who are more likely to benefit from or experience a certain outcome from a particular therapy. Predictive biomarkers provide extensive information on the probability of response patients will have to a specific type of therapy, whether positive or negative, and are essential for healthcare professionals and those in scientific fields. The probability of survival depends on treatment in patients who express the biomarker associated with a response to a particular therapy. In oncology and other medical fields, predictive biomarkers are used to tailor therapies for better outcomes.
How Predictive Biomarkers Are Used
Predictive biomarkers are used for:
- Identifying the most likely response to treatment: Predictive biomarkers help determine which patients are most likely to respond to a particular therapy. For example, HER2 (Human Epidermal Growth Factor Receptor 2) is a biomarker used in breast cancer to determine whether a patient will benefit from HER2-targeted therapies like trastuzumab (Herceptin).
- Predicting treatment outcomes: These biomarkers provide insights into how a patient’s disease may progress under a given treatment. For instance, KRAS mutations in colorectal cancer predict resistance to anti-EGFR (epidermal growth factor receptor) therapies, helping oncologists select more effective treatments.
- Improving and customizing treatment options: By analyzing predictive biomarkers, clinicians can refine and adjust treatment strategies for individual patients. For example, PD-L1 expression levels in non-small cell lung cancer (NSCLC) help determine whether a patient is a good candidate for immune checkpoint inhibitors like pembrolizumab (Keytruda).
- Personalizing medicine: Predictive biomarkers are at the core of personalized medicine, ensuring treatments are tailored to an individual’s genetic profile and disease characteristics. This minimizes trial-and-error approaches and reduces the risk of adverse effects. BRAF mutations in melanoma, for instance, guide the use of targeted therapies like vemurafenib.
Predictive Biomarkers for Precision Oncology
Predictive biomarkers are essential for precision oncology, enabling healthcare professionals to determine which patients are most likely to benefit from specific treatments. By guiding targeted therapies, these biomarkers help create personalized treatment plans that improve patient outcomes, minimize unnecessary side effects, and reduce overall treatment costs. As a result, precision oncology is transforming cancer care by moving away from a one-size-fits-all approach toward more effective, individualized treatment strategies.
Challenges of Predictive Biomarker Discovery & Validation
Despite the potential of predictive biomarkers to revolutionize personalized medicine in oncology and other fields, their discovery and validation come with significant challenges:
- Biological Complexity: Diseases are often influenced by multiple genetic, environmental, and molecular factors, making it difficult to isolate a single reliable biomarker.
- Data Variability: Biomarker studies rely on biological samples that can vary based on genetics, sample collection methods, and patient conditions, leading to inconsistent results.
- Reproducibility Issues: Many biomarkers fail during validation because their predictive power cannot be consistently replicated across different populations or clinical settings.
- Regulatory and Approval Hurdles: To gain clinical acceptance, biomarkers must pass rigorous analytical validation, clinical validation, and utility assessments, which can be time-consuming and costly.
- Integration with Existing Diagnostics: Even if a biomarker is validated, integrating it into current diagnostic frameworks and treatment protocols can be complex and require additional clinical evidence.
Addressing these challenges requires advancements in multi-omics technologies, AI-driven data analysis, and standardized validation protocols to improve reliability and clinical adoption.
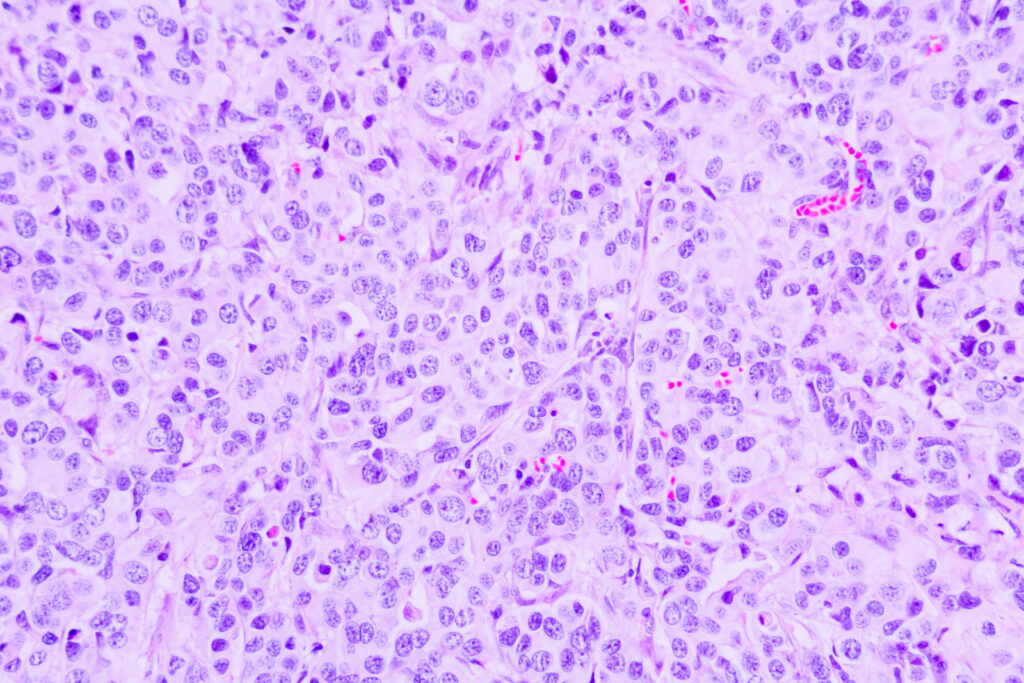
Do You Need FFPE Tissue Samples for Predictive Biomarker Testing?
When performing predictive biomarker testing, it’s crucial to have high-quality tissue samples available. Superior BioDiagnostics understands this, and we provide a range of normal and malignant/disease-state FFPE tissue samples for your analysis. Our tissue samples are ethically sourced and 100% US procured, ensuring top quality.
Our biospecimen samples are customized to meet your specific needs, and we offer next-day shipping to ensure you receive essential results without delay. Order from Superior BioDiagnostics to perform predictive biomarker testing for oncology, neurology, cardiology, and other fields. Contact our team if you have any questions; we’ll gladly assist you.
